Introduction
The female reproductive system consists of internal and external organs. It creates hormones and is responsible for fertility, menstruation and sexual activity.
The female reproductive system is the body parts that help women or people assigned female at birth (AFAB):
Have sexual intercourse.
Reproduce.
Menstruate.
Anatomy
The female reproductive anatomy includes both external and internal parts.
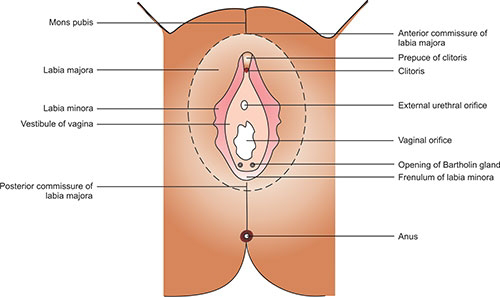
External parts
The function of your external genitals are to protect the internal parts from infection and allow sperm to enter your vagina.
Your vulva is the collective name for all your external genitals. A lot of people mistakenly use the term “vagina” to describe all female reproductive parts. However, your vagina is its own structure located inside your body.
The main parts of your vulva or external genitals are:
Labia majora: Your labia majora (“large lips”) enclose and protect the other external reproductive organs. During puberty, hair growth occurs on the skin of the labia majora, which also contain sweat and oil-secreting glands.
Labia minora: Your labia minora (“small lips”) can have a variety of sizes and shapes. They lie just inside your labia majora, and surround the opening to your vagina (the canal that joins the lower part of your uterus to the outside of your body) and urethra (the tube that carries pee from your bladder to the outside of your body). This skin is very delicate and can become easily irritated and swollen.
Clitoris: Your two labia minora meet at your clitoris, a small, sensitive protrusion that’s comparable to a penis in men or people assigned male at birth (AMAB). Your clitoris is covered by a fold of skin called the prepuce and is very sensitive to stimulation.
Vaginal opening: Your vaginal opening allows menstrual blood and babies to exit your body. Tampons, fingers, sex toys or penises can go inside your vagina through your vaginal opening.
Hymen: Your hymen is a piece of tissue covering or surrounding part of your vaginal opening. It’s formed during development and present during birth.
Opening to your urethra: The opening to your urethra is the hole you pee from.
Internal parts
Vagina: Your vagina is a muscular canal that joins the cervix (the lower part of uterus) to the outside of the body. It can widen to accommodate a baby during delivery and then shrink back to hold something narrow like a tampon. It’s lined with mucous membranes that help keep it moist.
Cervix: Your cervix is the lowest part of your uterus. A hole in the middle allows sperm to enter and menstrual blood to exit. Your cervix opens (dilates) to allow a baby to come out during a vaginal childbirth. Your cervix is what prevents things like tampons from getting lost inside your body.
Uterus: Your uterus is a hollow, pear-shaped organ that holds a fetus during pregnancy. Your uterus is divided into two parts: the cervix and the corpus. Your corpus is the larger part of your uterus that expands during pregnancy.
Ovaries: Ovaries are small, oval-shaped glands that are located on either side of your uterus. Your ovaries produce eggs and hormones.
Fallopian tubes: These are narrow tubes that are attached to the upper part of your uterus and serve as pathways for your egg (ovum) to travel from your ovaries to your uterus. Fertilization of an egg by sperm normally occurs in the fallopian tubes. The fertilized egg then moves to the uterus, where it implants into your uterine lining.
Functions
The female reproductive system provides several functions. In addition to allowing a person to have sexual intercourse, it also helps a person reproduce.
Your ovaries produce eggs. These eggs are then transported to your fallopian tube during ovulation where fertilization by a sperm may occur. The fertilized egg then moves to your uterus, where the uterine lining has thickened in response to the normal hormones of your menstrual cycle (also called your reproductive cycle). Once in your uterus, the fertilized egg can implant into the thickened uterine lining and continue to develop. If implantation doesn’t take place, the uterine lining is shed as your menstrual period. In addition, the female reproductive system produces sex hormones that maintain your menstrual cycle.
During menopause, the female reproductive system gradually stops making the female hormones necessary for the menstrual cycle to work. At this point, menstrual cycles can become irregular and eventually stop. You’re considered to be menopausal when you’ve gone an entire year without a menstrual period.
Menstrual cycle
Women or people AFAB of reproductive age (beginning anywhere from 11 to 16 years of age) experience cycles of hormonal activity that repeat at about one-month intervals. With every cycle, your body prepares for a potential pregnancy, whether or not that’s your intention. The term menstruation refers to the periodic shedding of your uterine lining when pregnancy doesn’t occur that cycle. Many people call the days that they notice vaginal bleeding their “period.”
The average menstrual cycle takes about 28 days and occurs in phases. These phases include:
The follicular phase (the egg develops).
The ovulatory phase (release of the egg).
The luteal phase (hormone levels decrease if the egg doesn’t implant).
There are four major hormones (chemicals that stimulate or regulate the activity of cells or organs) involved in the menstrual cycle. These hormones include:
Follicle-stimulating hormone.
Luteinizing hormone.
Estrogen.
Progesterone.
Follicular phase
This phase starts on the first day of your period. During the follicular phase of the menstrual cycle, the following events occur:
Two hormones, follicle stimulating hormone (FSH) and luteinizing hormone (LH) are released from your brain and travel in your blood to your ovaries.
The hormones stimulate the growth of about 15 to 20 eggs in your ovaries, each in its own “shell,” called a follicle.
These hormones (FSH and LH) also trigger an increase in the production of the hormone estrogen.
As estrogen levels rise, like a switch, it turns off the production of follicle-stimulating hormone. This careful balance of hormones allows the body to limit the number of follicles that will prepare eggs to be released.
As the follicular phase progresses, one follicle in one ovary becomes dominant and continues to mature. This dominant follicle suppresses all of the other follicles in the group. As a result, they stop growing and die. The dominant follicle continues to produce estrogen.
Ovulatory phase
The ovulatory phase (ovulation) usually starts about 14 days after the follicular phase started (the exact timing varies). The ovulatory phase is the second phase of your menstrual cycle. Most people will have a menstrual period 10 to 16 days after ovulation. During this phase, the following events occur:
The rise in estrogen from the dominant follicle triggers a surge in the amount of luteinizing hormone (LH) that your brain produces.
This causes the dominant follicle to release its egg from the ovary.
As the egg is released (a process called ovulation) it’s captured by finger-like projections on the end of the fallopian tubes (fimbriae). The fimbriae sweep the egg into the fallopian tube.
For one to five days prior to ovulation, many women or people AFAB will notice an increase in egg white cervical mucus. This mucus is the vaginal discharge that helps to capture and nourish a sperm on its way to meet the egg for fertilization.
Luteal phase
The luteal phase begins right after ovulation and involves the following processes:
Once it releases its egg, the empty ovarian follicle develops into a new structure called the corpus luteum.
The corpus luteum secretes the hormones estrogen and progesterone. Progesterone prepares your uterus for a fertilized egg to implant.
If intercourse has taken place and sperm has fertilized the egg (conception), the fertilized egg (embryo) will travel through your fallopian tube to implant in your uterus. This is how pregnancy begins.
If the egg isn’t fertilized, it dissolves in your uterus. Not needed to support a pregnancy, the lining of your uterus breaks down and sheds. This is when your period begins.
Eggs
You’re born with all the eggs you’ll ever produce. During fetal development, you have about 6 million eggs. At birth, there are approximately 1 million eggs left. By the time you reach puberty, only about 300,000 remain. The number of eggs you have continues to decline as you age and menstruate each cycle. Fertility also declines with age due to the decreasing number and quality of your remaining eggs.
Reproduction
In humans, female and male reproductive systems work together to reproduce. There are two kinds of sex cells — sperm and eggs. When a sperm meets an egg, it can fertilize it and create a zygote. This zygote eventually becomes a fetus. Both a sperm and an egg are needed for human reproduction.
Disease
Endometriosis
Endometriosis is a problem affecting a woman’s uterus—the place where a baby grows when a woman is pregnant. Endometriosis is when the kind of tissue that normally lines the uterus grows somewhere else. It can grow on the ovaries, behind the uterus, on the bowels, or on the bladder. Rarely, it grows in other parts of the body.
This “misplaced” tissue can cause pain, infertility, and very heavy periods. The pain is usually in the abdomen, lower back, or pelvic areas. Some women have no symptoms at all, and having trouble getting pregnant may be the first sign they have endometriosis.
Uterine Fibroids
Uterine fibroids are the most common noncancerous tumors in women of childbearing age. Fibroids are made of muscle cells and other tissues that grow in and around the wall of the uterus, or womb. The cause of fibroids is unknown. Risk factors include being African-American or being overweight. The symptoms of fibroids include
Heavy or painful periods or bleeding between periods.
Feeling “full” in the lower abdomen.
Urinating often.
Pain during sex.
Lower back pain.
Reproductive problems, such as infertility, multiple miscarriages, or early labor.
But some women will have no symptoms. That is why it is important to see your health care provider for routine exams.
Gynecologic Cancers
CDC provides information and educational materials for women and health care providers to raise awareness about the five main gynecologic cancers. Gynecologic cancer is any cancer that starts in a woman’s reproductive organs. Gynecologic cancers begin in different places within a woman’s pelvis, which is the area below the stomach and in between the hip bones.
Cervical cancer begins in the cervix, which is the lower, narrow end of the uterus.
Ovarian cancer begins in the ovaries, which are located on each side of the uterus.
Uterine cancer begins in the uterus, the pear-shaped organ in a woman’s pelvis where the baby grows when a woman is pregnant.
Vaginal cancer begins in the vagina, which is the hollow, tube-like channel between the bottom of the uterus and the outside of the body.
Vulvar cancer begins in the vulva, the outer part of the female genital organs.
HIV
HIV is the human immunodeficiency virus. HIV affects specific cells of the immune system (called CD4 cells). Over time, HIV can destroy so many of these cells that the body can’t fight off infection anymore. The human body cannot get rid of HIV—that means once a person has HIV, he or she has it for life. There is no cure at this time, but with proper medical care, the virus can be controlled. HIV is the virus that can lead to acquired immune deficiency syndrome, or AIDS. AIDS is the late stage of HIV infection, when a person’s immune system is severely damaged.
HIV in Women
Women who are infected with HIV typically get it by having sex with a man who is infected or by sharing needles with an infected person. Women of minority races/ethnicities are especially affected, and black or African American women are the most affected group.
Pregnant Women
All pregnant women should know their HIV status. Pregnant women who are HIV-positive can work with their health care providers to ensure their babies do not contract HIV during pregnancy, delivery, or after delivery (through breast milk). It is possible for a mother to have HIV and not spread it to her baby, especially if she knows about her HIV status early and works with her health care provider to reduce the risk.
Learn more from CDC’s Act Against AIDS campaign including how HIV is spread, and how to prevent HIV.
Interstitial cystitis
Interstitial cystitis (IC) is a chronic bladder condition resulting in recurring discomfort or pain in the bladder or surrounding pelvic region. People with IC usually have inflamed or irritated bladder walls that can cause scarring and stiffening of the bladder. IC can affect anyone; however, it is more common in women than men. Some people have some or none of the following symptoms:
Abdominal or pelvic mild discomfort.
Frequent urination.
A feeling of urgency to urinate.
Feeling of abdominal or pelvic pressure.
Tenderness.
Intense pain in the bladder or pelvic region.
Severe lower abdominal pain that intensifies as the urinary bladder fills or empties.
Polycystic Ovary Syndrome PCOS
Polycystic ovary syndrome happens when a woman’s ovaries or adrenal glands produce more male hormones than normal. One result is that cysts (fluid-filled sacs) develop on the ovaries. Women who are obese are more likely to have PCOS. Women with PCOS are at increased risk of developing diabetes and heart disease. Symptoms may include
Infertility.
Pelvic pain.
Excess hair growth on the face, chest, stomach, thumbs, or toes.
Baldness or thinning hair.
Acne, oily skin, or dandruff.
Patches of thickened dark brown or black skin.
STDs
STDs are infections that you can get from having sex with someone who has the infection. The causes of STDs are bacteria, parasites, and viruses. There are more than 20 types of STDs. Read more about specific STDs from these CDC fact sheets.
Most STDs affect both men and women, but in many cases the health problems they cause can be more severe for women. If a pregnant woman has an STD, it can cause serious health problems for the baby.
If you have an STD caused by bacteria or parasites, your health care provider can treat it with antibiotics or other medicines. If you have an STD caused by a virus, there is no cure, but antiviral medication can help control symptoms. Sometimes medicines can keep the disease under control. Correct usage of latex condoms greatly reduces, but does not completely eliminate, the risk of catching or spreading STDs.