Zoology
Myself Tamilvanan S S M. Sc., (Zoology) B. Ed.,
Saturday, May 25, 2024
Reverse Transcription
Monday, April 8, 2024
Erythroblastosis Fetalis
Carbon-14 Dating
Carbon-14 Dating
Introduction
Radiocarbon dating, or carbon-14 dating, is a scientific method that can accurately determine the age of organic materials as old as approximately 60,000 years. First developed in the late 1940s at the University of Chicago by Willard Libby, the technique is based on the decay of the carbon-14 isotope. Radiocarbon dating has been used for historical studies and atmospheric science, and triggered archaeology’s “Radiocarbon Revolution.”
Carbon-14 dating
The invention of radiocarbon dating elegantly merged chemistry and physics to develop a scientific method that can accurately determine the age of organic materials as old as approximately 60,000 years.
It is based on the fact that living organisms—like trees, plants, people, and animals—absorb carbon-14 into their tissue. When they die, the carbon-14 starts to change into other atoms over time. Scientists can estimate how long the organism has been dead by counting the remaining carbon-14 atoms. The technique was developed in the late 1940s at the University of Chicago by chemistry professor Willard Libby, who would later receive the Nobel Prize for the work.
The breakthrough introduced a new scientific rigor to archaeology, allowing archaeologists to put together a history of humans across the world, but it had a significant effect in other fields, too.
Carbon dating has helped us reveal how our bodies work, to understand the climate of the Earth and reconstruct its history, and to track the sun’s activity and the Earth’s magnetic fields. Radiocarbon dating was also instrumental in the discovery of human-caused climate change, as scientists used it to track the sources of carbon in the atmosphere over time.
Radiocarbon dating working principle
It starts with cosmic rays—subatomic particles of matter that continuously rain upon Earth from all directions. When cosmic rays reach Earth’s upper atmosphere, physical and chemical interactions form the radioactive isotope carbon-14.
Living organisms absorb this carbon-14 into their tissue. Once they die, the absorption stops, and the carbon-14 begins very slowly to change into other atoms at a predictable rate. By measuring how much carbon-14 remains, scientists can estimate how long a particular organic object has been dead.
From there, the problem becomes how to measure the carbon-14. Libby and fellow chemists at the University of Chicago and other institutions developed techniques to purify a sample so that it emits no other type of radiation except for carbon-14, and then run it through a detector sensitive enough to accurately count the pings emitted by the decay of single atoms. A newer, faster method developed in the 1970s works by using a particle accelerator to count the atoms of carbon-14.
Radiocarbon dating can be used on any object that used to be alive. That includes pieces of animals, people, and plants, but also paper that was made from reeds, leather made from animal hides, logs that were used to build houses, and so forth.
Carbon Dating Invention
Carbon dating was invented in the late 1940s by Willard Libby, a chemistry professor at the University of Chicago and former Manhattan Project scientist.
Libby built upon the work of Martin Kamen (PhD’36) and Sam Ruben, who discovered the carbon-14 isotope in 1940. Carbon-14 has a half-life of about 5,730 years. That means half the atoms in a sample will change into other atoms, a process known as “decay,” in that amount of time.
Libby proposed the idea of carbon dating in the journal Physical Review in 1946. He further developed the concept with members of his research group and published more in Science in 1947 and 1949.
In a crucial step, Libby’s first graduate student, Ernest C. Anderson, established that organic materials contained essentially the same natural abundance of radiocarbon at all measured latitudes reaching nearly from pole to pole.
Libby worked with colleagues, including anthropologist Robert Braidwood of UChicago’s Oriental Institute (now known as the Institute for the Study of Ancient Cultures), to develop the carbon-14 method.
Samples taken from artifacts in the museum collections were used to test the accuracy of radiocarbon dating, since archaeologists already knew their ages by tree-ring dating and other evidence.
The many materials Libby tested while developing the method included a rope sandal found in an Oregon cave, the dung of an extinct ground sloth, linen wrappings from the Dead Sea Scrolls, and part of a funeral ship deck placed in the tomb of Sesostris III of Egypt.
News of the technique spread rapidly. By 1960, more than 30 radiocarbon labs had been established worldwide. (One of the first was led by physicist Hilde Levi, who spent several months at UChicago working with Libby on radiocarbon-related problems in 1947 and 1948).
“Libby’s method remained the only way to measure carbon-14 in samples for several decades and was long considered the most accurate means of dating carbon decay,” said David Mazziotti, a UChicago professor in chemistry. (Today, scientists also use a different way to measure carbon-14 called accelerator mass spectrometry, which can get more precise results from a far smaller amount of sample but is more expensive).
A plaque in the foyer of UChicago’s Kent Laboratory building commemorates the discovery, as a National Historic Chemical Landmark designated by the American Chemical Society. Libby’s invention earned him the 1960 Nobel Prize in chemistry “for determinations in archaeology, geology, geophysics, and other branches of science.”
UChicago science historian Emily Kern has documented how radiocarbon dating developed in an unusual Cold War context. She described how the technique developed into a wide-ranging, global network from a technology that had roots in World War II’s Manhattan Project to build the atomic bomb. The technology, unbound by national security concerns, meant that carbon-14 laboratories could arise in Australia, Denmark, New Zealand and elsewhere.
Limitations of Carbon-14 Dating
The various dating techniques all have limitations. Each works best for different types of problems. Radiocarbon dating works on organic materials up to about 60,000 years of age.
Conventional radiocarbon dating requires samples of 10 to 100 grams (0.35 to 3.5 ounces) of an object, depending on the material in question. Newer forms of dating can use much smaller amounts, down to 20 to 50 milligrams or 0.0007 to 0.0018 ounces. In both cases, the material is destroyed during the test.
Radiocarbon samples are also easily contaminated, so to provide accurate dates, they must be clean and well-preserved. Dirt and other matter must be washed off with water, but chemical treatments and other cleaning procedures are also often needed.
This is because there are so few atoms to count; even a little extra carbon from contamination will throw off the results significantly. A million-year-old sample contaminated by only a tiny amount of carbon could yield an invalid age of 40,000 years, for example.
Other dating methods have different strengths. Dendrochronology, also known as tree-ring dating, depends upon the preservation of certain tree species; it can extend to about 12,500 years ago for oak trees and to 8,500 years for bristlecone pine.
Potassium-argon dating can date volcanic materials ranging from less than 100,000 to more than 4 billion years old. Rubidium-strontium dating can be used to determine the ages of items ranging from a few million to a few billions of years old; it is widely used to understand how the Earth and solar system formed and to trace human migration and trade in archaeology.
Improved version
Technological and analytical advances have made radiocarbon dating faster and much more precise—and expanded its range of uses by reducing the size of the sample needed. The latest form of radiocarbon dating, called accelerator mass spectrometry, needs samples of only 20 to 50 milligrams (0.0007 to 0.0018 ounces); however, it is also more expensive.
Another newer development is Bayesian statistical modeling, which applies probability analytics to radiocarbon dates, which always involve an error margin. Bayesian modeling hones the final date range by considering factors such as which layer of sediments the samples come from or their relationship to artifacts of known age.
Discoveries that carbon-14 testing Revealed
Since its discovery, carbon-14 testing has had a major impact on our understanding of fields from archaeology to history to geology.
Dual Process Theory - Psychology
Bipolar Disorder
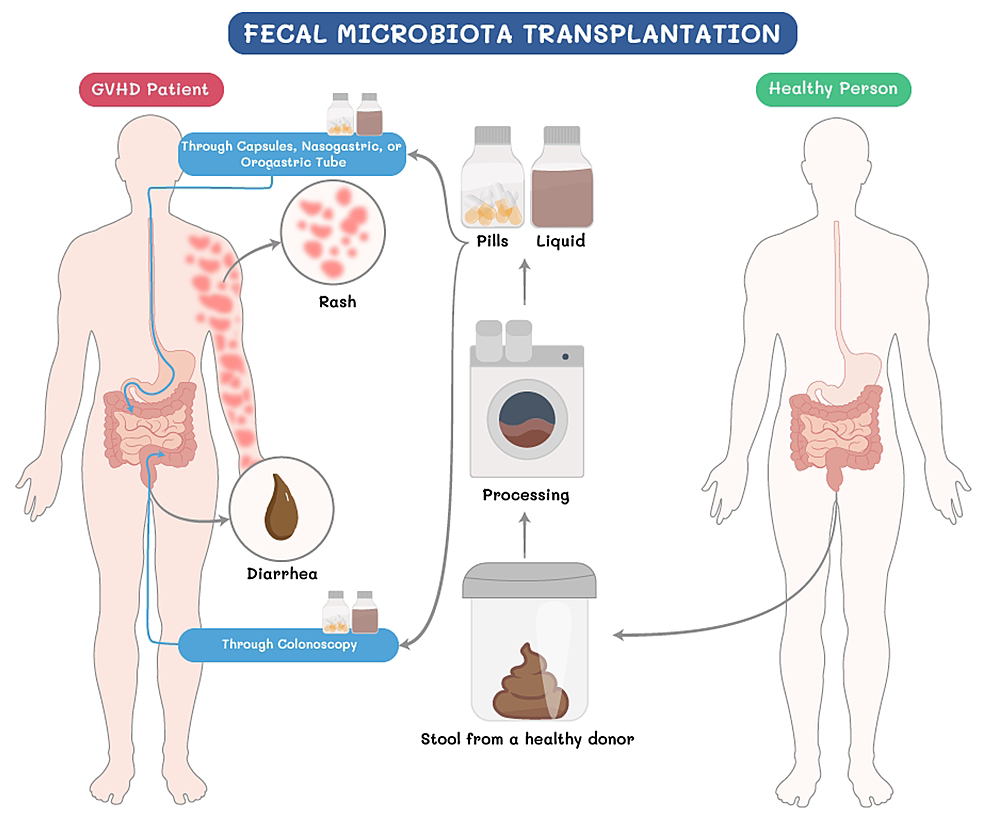
Fecal Microbiota Transplantation (FMT)
Blood– Brain Barrier (BBB)
Gut - Brain Axis (GBA)
Autism Spectrum
Dementia
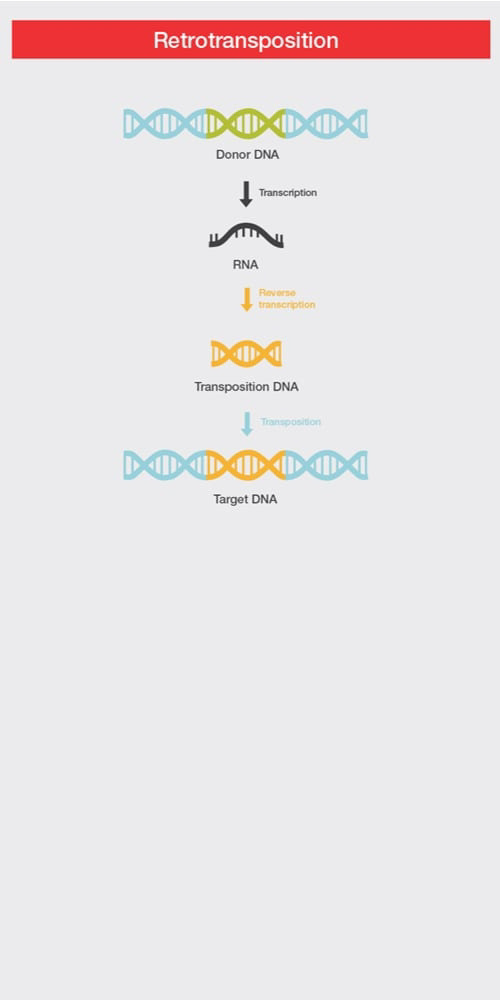
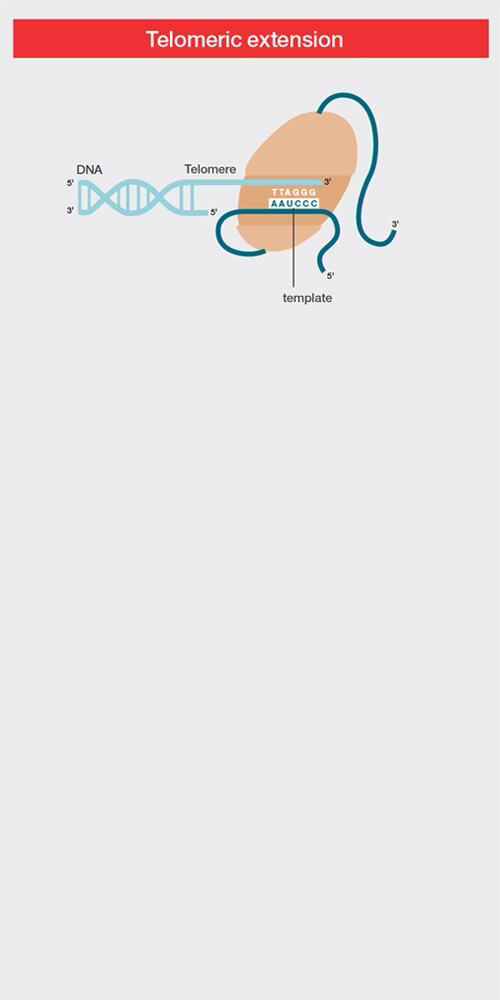
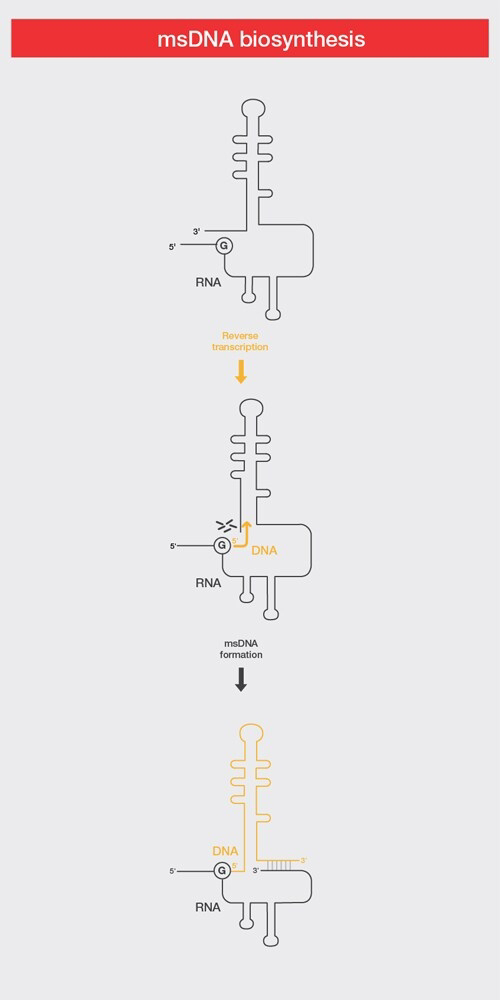
Reverse Transcription
Reverse Transcription Introduction Reverse transcription is the synthesis of DNA from an RNA template. This process is driven by RNA-depende...

-
Rocket Immunoelectrophoresis Introduction Rocket Immunoelectrophoresis is an adaptation of radial immunodiffusion developed by L...
-
Erythroblastosis Fetalis Introduction The adult human body is home to trillions of red blood cells, also known as RBCs or erythrocytes. Thes...
-
Reverse Transcription Introduction Reverse transcription is the synthesis of DNA from an RNA template. This process is driven by RNA-depende...